Understanding Cytolytic Vaginosis (CV): Causes, Symptoms, and Effective Solutions
Besides bacterial vaginosis, there is another “vaginosis.”
You might be familiar with bacterial vaginosis (BV). In medical terms, "vaginosis" refers to vaginal dysbiosis, which indicates an imbalance in the vaginal microbiome, also known as the vaginal microbiota or vaginal flora.
BV-related dysbiosis occurs due to a decrease in the population of beneficial Lactobacillus bacteria typically found in the vagina and an overgrowth of anaerobic bacteria, such as Gardnerella vaginalis.

Common signs and symptoms of BV include a fishy odor, unusual vaginal discharge, elevated vaginal pH, vaginal itching, burning, and discomfort during sexual intercourse.
However, did you know that there is another type of vaginosis? This condition also leads to excessive vaginal discharge, itching, burning, and discomfort during sex. However, unlike BV, it does not result in a fishy odor or an increase in vaginal pH.
What is cytolytic vaginosis?
This other vaginosis is called cytolytic vaginosis (CV), Lactobacillus overgrowth syndrome or Doderlein’s cytolysis. The overgrowth of vaginal lactobacillus bacteria produces increased amount of lactic acid, which causes the vaginal epithelial cells (the vaginal lining skin that covers the vaginal wall) to lyse (break down) and peel off to form discharge. Thus, this condition is called "cytolytic vaginosis."
This condition is less common than BV and yeast (vulvovaginal candidiasis or vaginal thrush). Thus, it is lesser known. It can cause similar symptoms and is often misdiagnosed as yeast or BV.

Some women with CV (Cytolytic Vaginosis) initially undergo treatment for yeast or BV (Bacterial Vaginosis). However, if these treatment attempts repeatedly prove unsuccessful, their doctors may reevaluate their conditions.
Upon reexamination, when doctors observe that these women have an increased population of vaginal Lactobacillus bacteria and their vaginal pH is either normal or lower than normal, the condition is diagnosed as CV.
What causes CV?
Cytolytic is derived from cytolysis, which refers to the breakdown of cells. In cases where an excessive amount of lactic acid washes away the shed vaginal lining cells, the underlying vaginal wall tissue is left exposed without its usual protective covering. This condition is somewhat similar to desquamative inflammatory vaginitis, resulting in heightened sensitivity to irritation in the vagina, leading to itching, burning, and discomfort.
The factors responsible for the overgrowth of vaginal lactobacillus bacteria remain unknown. However, certain factors, such as recent antibiotic use, the use of high-strength probiotics, or antifungal medications, may contribute to the development of CV.
Interestingly, some women have reported experiencing CV after taking the prebiotic lactulose.

Lactulose is a prebiotic that specifically nourishes lactobacilli species in the vagina, potentially leading to an overabundance of lactobacillus species. This overgrowth can result in cytolytic vaginosis (CV), a condition that typically resolves on its own once the consumption of lactulose is discontinued. However, for some women, CV does not spontaneously resolve even after they stop using lactulose.
What are the symptoms?
An excess of acid produced due to the overgrowth of Lactobacillus bacteria can lead to irritation and vaginal discharge. This discharge does not typically have a strong odor, especially not a fishy odor. However, it shares some similarities in symptoms with other conditions such as vulvovaginal candidiasis (yeast infection), bacterial vaginosis (BV), or vaginal trichomoniasis caused by Trichomonas vaginalis (trich). These shared symptoms include the presence of excessive white and thick discharge, itching, burning, irritation, and discomfort during sexual intercourse.
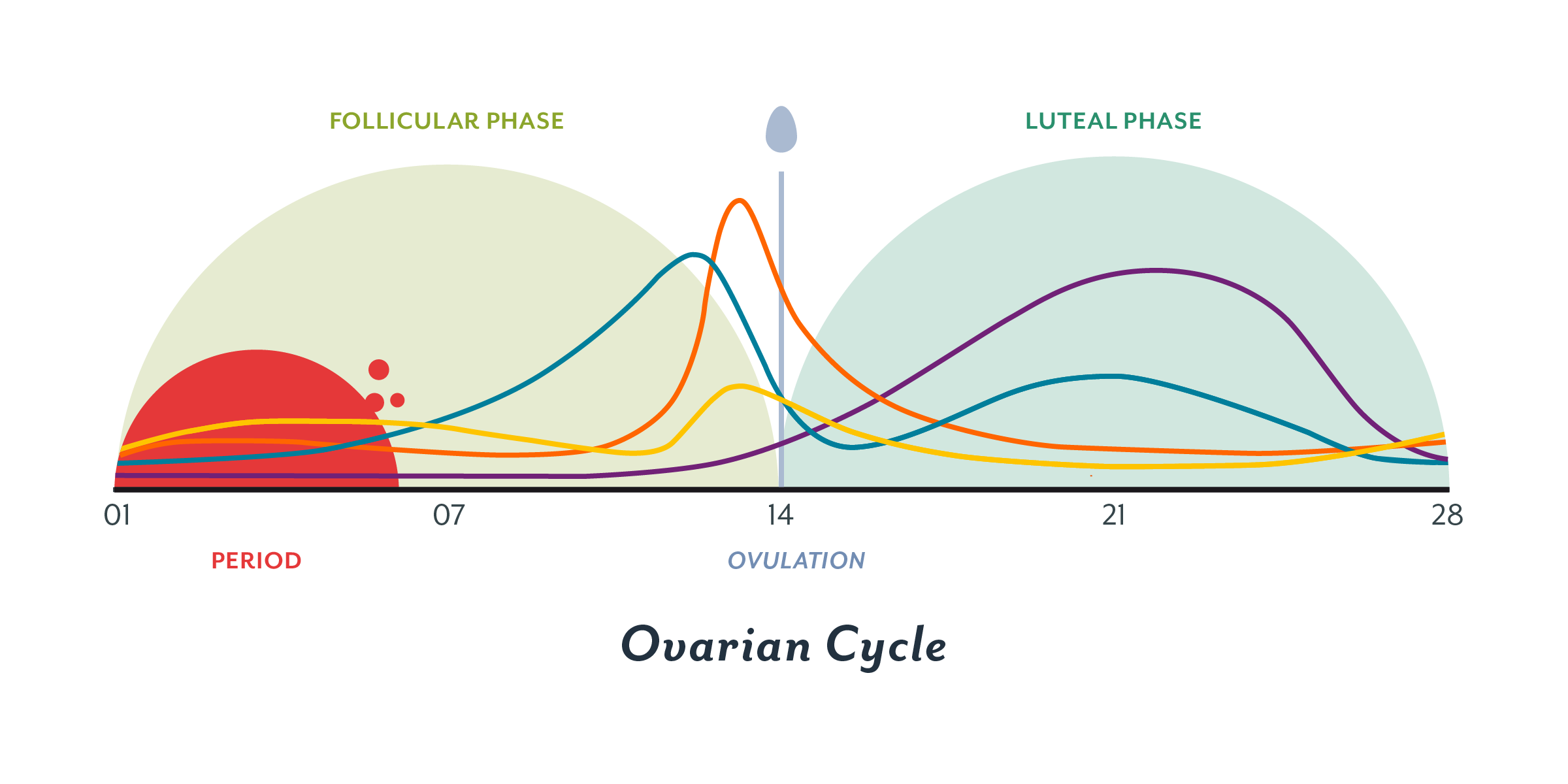
Symptoms often worsen during the luteal phase of the menstrual cycle just before menstruation begins. Menstrual flow can help alleviate these symptoms because the menstrual blood assists in diluting or flushing out the acid produced by the excessively growing lactobacillus bacteria.
To draw a parallel, you may recall occasional experiences of gastric juice regurgitating into your mouth, resulting in a very sour taste. This gastric acid reflux can cause irritation and discomfort.
Fortunately, instances of acid reflux into the mouth are infrequent and brief, allowing you to easily either spit out the acid or swallow it back down. A simple rinse with water helps remove any residual gastric acid. In contrast, Gastro-Esophageal Reflux Disease, or GERD for short, involves regular and chronic acid reflux.
Regrettably, for women with CV, the excessive lactic acid production is akin to GERD. This acid is consistently produced and does not dissipate easily, potentially causing ongoing irritation and discomfort within the vagina.
Who may get CV?
The female hormone estrogen plays a crucial role in supporting the synthesis of glycogen in vaginal cells. As these cells shed, glycogen is released to facilitate the growth of vaginal lactobacilli. Therefore, a prerequisite for CV is having a high estrogen level. Consequently, CV typically affects women in their reproductive age, typically between 15 and 45 years old.
Prepubescent girls and postmenopausal women are less likely to experience CV due to their lower estrogen levels. However, there is an exception: postmenopausal women who undergo hormone replacement therapy or bioidentical hormone treatment may still develop CV because these treatments restore estrogen levels that naturally decline after menopause.
In summary, two key factors, age and hormone supplementation, can help determine whether vaginal discomfort is caused by CV or not.

Conversely, if you are taking estrogen supplements and experiencing CV, it could indicate that you might be taking an excessive amount of estrogen. Gradually reducing your estrogen supplement intake may allow CV to heal naturally. It's worth noting that estrogen supplementation can also elevate the risk of certain cancers. Therefore, it may be beneficial for your overall health to taper off estrogen supplementation, even if you do not have CV. You can find guidance on how to do this in the following resource.
How is CV diagnosed?
Cytolytic vaginosis is almost always misdiagnosed at first as yeast or BV because their symptoms are very much alike.

However, after using different antifungal and/or antibiotic drugs, or self-care products failed to clear the discharges and other discomforts, CV may be suspected.

A gynecologist may conduct a laboratory test or examine a Pap smear or a wet slide under a microscope. When the doctor observes a significant presence of Lactobacillus bacteria, a diagnosis of cytolytic vaginosis can be made. To further confirm the microscopic diagnosis, a DNA test, such as Juno, may be employed.
What are unique features of CV?
Cytolytic Vaginosis (CV) shares many common features with yeast infections, BV, and trichomoniasis, including symptoms like discharges, itching, burning, and painful intercourse. However, it also possesses several distinctive characteristics:
- Yeast or Trichomonas vaginalis is absent in the culture test or under the microscopy.
- Lactobacillus bacteria are abundant in the smear.
- Vaginal pH is low at 3.5 - 4.5. Yeast: pH 4.0-5.0; BV: pH >5.0
- Discharge is odorless (no rotten fishy odor or any unpleasant odor)
- Cyclic symptoms: worsen in the luteal phase of the menstrual cycle before the menstrual period, relieve during menstruation (menstrual blood dilutes and flushes acid out), reappear after menstruation.
- Common Lactobacillus species found in CV in the lab test may include L. crispatus, L. gasseri, and L. jensenii.
A doctor's expertise is required to examine and diagnose conditions such as yeast infections, trichomoniasis, BV, and the presence of Lactobacillus bacteria. However, you can perform simple self-assessments to check for vaginal pH levels and odor.
If you've previously been diagnosed with yeast or BV and have tried various treatment products without success, it may be worth considering the possibility of CV. You can measure your vaginal pH and assess whether your vaginal discharge exhibits a fishy odor as part of this self-assessment.
How to measure vaginal pH?
You can find several different pH testing kits designed for testing vaginal pH on Amazon. These kits have two basic components: pH paper strips and a color chart with corresponding pH values. Some kits may also include Q-tips, but most do not as Q-tips are a common household item.

We recommend this Pelvana brand because it is easier to read. Other brands are cheaper but may be a waste of money because it is hard to separate their colors of pH 4.5 and pH 5.0.
To measure vaginal pH, insert a Q-tip into the vagina and hold it against the wall of your vagina for five seconds to allow it to absorb moisture. Withdraw the wet Q-tip and press it against the pH paper strip until it is fully wet.
Wait for a few minutes for the color on the pH paper strip to develop. This step may take up to five minutes, depending on the kit. Compare the color of your pH paper strip to the colors on the chart. Write down the number.
Note, you must compare the color while the paper strip is wet. After it becomes dry, the color changes and it may no longer be accurate.
If your pH is below 4.5, you may rule out BV as BV often has a higher pH. But you cannot rule out yeast yet.

How to check vaginal odor?
A typical symptom of BV is an unpleasant fishy odor.
If your discomfort is caused by BV, you may smell an odor like rotten fish. The odor is so bad that you may never forget about it. The odor will make your underwear smell too, and you cannot hide it.
Since CV does not have an odor, you can check the smell with a Q-tip.
Once you sample your vaginal secretion with the Q-tip, you can smell it for the presence of any odor. If you do not smell anything unpleasant, you do not have a BV-associated fishy odor.

If you have a pH below 4.5 and you do not smell fishy odor, your condition may not be BV.
Can discharge tell CV apart from yeast?
A yeast infection can sometimes present with a low pH but without an apparent odor. Therefore, it's important to consider other factors to rule out yeast as the cause.
Both CV and yeast infections can result in vaginal discharge. Women with CV often experience thick, white, or clumpy cottage cheese-like discharge, which can resemble the discharge seen in yeast infections. Consequently, relying solely on discharge as a symptom cannot reliably distinguish CV from yeast.
In a doctor's office, when examining vaginal secretions under a microscope, CV typically does not show the presence of white blood cells, which are involved in immune responses. In contrast, the vaginal secretions of women with yeast infections do contain white blood cells. Additionally, CV does not typically feature typical yeast cells in the discharge, whereas yeast infections may exhibit candida yeast cells. However, a doctor's expertise is often necessary to provide an accurate diagnosis.
If your condition is indeed caused by yeast, you can find relief by using antifungal creams like Monistat-3 or boric acid alternatives. Additionally, you may consider reducing the yeast load in your gut by taking Reset and Rejoice supplements.

However, if it is caused by CV, it may not respond to antifungal treatment. This may be a good indicator to separate CV from yeast.
How to distinguish CV from vaginal lactobacillosis?
Vaginal lactobacillosis (VL) is caused by an overgrowth of a lactobacillus-related bacterial species, Leptothrix vaginalis. Its cell shape is an elongated filamentous rod, 3-5 times longer than that of a Lactobacillus cell.
Previously, it was thought to be a subtype of Lactobacillus acidophilus. It is now classified as Leptothrix vaginalis. It is a relative of Lactobacillus.
Its overgrowth produces increased amount of lactic acid, which causes damage to the vaginal lining cells similar to cytolytic damages seen in CV. Therefore, CV and VL have similar clinical symptoms.
Using Pap smear and a wet mount slide, the long-rod shaped Leptothrix vaginalis bacteria associated with VL can be observed under a microscope.

Cytolytic vaginosis (CV) and vaginal lactobacillosis (VL) are mostly considered together as the Lactobacillus overgrowth syndrome. Therefore, these two diseases are related and may be treated by same approaches.
CV and VL are often considered together as the Lactobacillus overgrowth syndrome. Therefore, these two conditions are related and may be treated by the same approaches.
How to distinguish CV from AV?
Aerobic vaginitis treatment (AV) is characterized by a decrease in vaginal lactobacillus along with the presence of vaginal atrophy and predominantly aerobic bacteria. The aerobic bacteria may include E. coli, Enterococcus, Streptococcus, Staphylococcus, and Klebsiella. The source of these bacteria may include fecal contamination, the bladder, skin, and intimate partner.
Since vaginal atrophy occurs mostly in postmenopausal women, women with AV are often older and postmenopausal. Conversely, to produce sufficient lactic acid in the vagina, women must have sufficient supply of vaginal glycogen, which is supported by sufficient estrogen. Therefore, to develop CV, women are often younger and premenopausal, except for older women who are on estrogen supplement.
The most convincing diagnosis is a lab test. Women with AV will show aerobic bacteria like E. coli, while women with CV will show dominant Lactobacillus species.
How to distinguish CV from lichen sclerosus?
How i cured my lichen sclerosus is a rare, chronic skin disorder, usually of the genital and anal areas. It causes small patches of skin to become thin and colorless. It occurs more often in women over 40 years of age.
Common signs and symptoms include:
- Redness
- Itching
- Discomfort or pain
- Smooth white patches on the skin
- Blotchy, wrinkled patches
- Tearing or bleeding
- In severe cases, bleeding, blistering or ulcerated sores
- Painful sex
A major difference is that lichen sclerosus does not show vaginal discharge, but CV commonly shows abnormal vaginal discharge.
Can I order a lab test to confirm CV diagnosis?
You can order a vaginal microbiome test from a company called Juno.
If the test result shows that your vaginal Lactobacillus species is dominant (could be one species or multiple species but collectively their percentage is over 95%) and you have CV-like symptoms such as discharge, itching and burning, but no fishy odor, you may have CV.
This test can help you confirm the CV diagnosis from a doctor's office if your doctor did not order a lab test.
The test costs about $150 per test. You may ask them if their test is covered by medical insurance, Medicare, Medicaid, or FSA/HSA account.
Juno has been very kind to give our customers a group discount.
Dr. Chang recommends that if you have AV, BV, or CV, please get a test before treatment, immediately after treatment, and 1-3 months after. The lab test will help you choose the right product and assess its treatment effect.
If you have predominantly Lactobacillus species (close to 100%) in the vaginal sample and you have discomforts like pain, irritation, burning, itching, and/or discharge, some may be cottage cheese like charge, you may have CV.
An exception with Lactobacillus iners
Lactobacillus iners is a bad apple in the family of Lactobacillus. It is often associated with an increased risk of vaginal infection. If you see a high number (>10%) of L. iners in your lab test, most likely you may have a vaginal dysbiosis like BV or AV. If the population of the total Lactobacillus is close to 100%, which includes L. iners in significant numbers (>10%), you may developed a special type of CV, L. iners-associated vaginal dysbiosis. L. iners secretes a cytolytic toxin called inerolysin that kills your vaginal lining skin cells and cause burning and discharge. This type of CV requires additional steps to clear.
How is CV treated?
Once diagnosed, there are no treatment products specifically for CV. Some doctors may prescribe antibiotics. Unfortunately, antibiotics are often ineffective. Overuse often causes yeast infection or BV.
CV is a relatively rare condition affecting women's vaginal health. The market is relatively small. There has not been a commercial self-care product dedicated to managing CV. In doctor’s offices, a commonly prescribed medication is Clindamycin cream. It can suppress the overgrowth of vaginal Lactobacillus bacteria to provide relief.
The antibiotics may be effective, but a problem with the antibiotic cream is that after vaginal lactobacillus bacteria are wiped out by the antibiotics, yeast infection may occur, similar to issues with bv treatment online.
Below are some self-care methods for managing CV:
- Avoid vaginal probiotics or foods containing Lactobacillus, like yogurt.
- Avoid certain prebiotics like lactulose. Lactulose is also used as an osmotic laxative that treats constipation and liver problems. If you have CV and need to use a laxative, avoid lactulose, and try other laxatives instead.
- Baking soda sitz bath.
- Baking soda douche.
- Baking soda capsules or tablets.
- Change tampon to pads for menstrual hygiene.

Warning: Although baking soda may provide temporary relief, repeated use may cause serious side effects that can be more harmful than CV itself.
Baking soda is around 8.4 on the pH scale, slightly above the neutral mark of 7. It may cause burning in some women. Repeated use or overuse of the baking soda capsules, tablets, douche or sitz bath may disrupt the vaginal microbiome and cause bacterial vaginosis (BV), yeast infection, and/or pelvic inflammatory disease (PID).
If you encounter any difficulty, we suggest that you consult with a doctor who understands CV. Since CV is relatively new and not well known to the medical community, not all doctors are familiar with CV and can help you find a best solution.
Does baking soda cause side effects?
Based on available literature, approximately half of women with Cytolytic Vaginosis (CV) may experience relief from their symptoms by using baking soda sitz baths or using baking soda capsules or tablets as vaginal inserts. Baking soda can elevate vaginal pH levels, alleviating symptoms related to the acidity associated with CV. However, it does not address the root cause of CV, which is the overgrowth of Lactobacillus bacteria. This might explain why approximately half of women with CV do not respond favorably to baking soda treatments.
 Baking soda can be easily overused to cause serious side effects.
Baking soda can be easily overused to cause serious side effects.
Baking soda is a mild base with a pH of 8.4. If used sparingly, its effects may be short-lived, and CV symptoms could return once its usage is discontinued. However, excessive use can lead to burning and irritation, particularly among women who are sensitive to such discomfort. In such cases, baking soda may prove ineffective due to inadequate use.
On the other hand, for women who are less sensitive to the irritation caused by baking soda, there's a risk of overuse, which can result in serious side effects. Overusing baking soda, despite experiencing irritation, can act as an antiseptic and potentially eliminate the normally protective vaginal Lactobacillus bacteria. Restoring a normal vaginal flora can be challenging once it is disrupted, and this disruption may lead to recurrent yeast infections or BV due to the absence of vaginal Lactobacillus bacteria.
Baking soda use may cause PID and infertility
Many women with CV have tried baking soda and got vulva burning and pelvic pain. The worst side effect may be from baking soda douche. The reason is that douching itself, regardless if you use baking soda or plain water, can cause serious health damages. The US government scientists at NIH and the entire medical community are against douching, because douching reduces woman's resistance to infections and have been linked to BV (bacterial vaginosis), PID (pelvic inflammatory disease), and STI (sexually transmitted infections).
Pelvic inflammatory disease or PID is an infection of the upper part of the female reproductive system, namely the uterus, fallopian tubes, and ovaries, and inside of the pelvis. Pelvic pain is the common symptom. If PID occurs, about 1-in-10 women develop infertility. It can be more difficult to manage and it is too great a health risk to take when there is a safer alternative for CV treatment.

It is currently unclear why the use of baking soda capsules, tablets, douches, or sitz baths may potentially lead to Pelvic Inflammatory Disease (PID). However, we can propose a plausible explanation.
Normally, Lactobacillus serves as the primary defense within a woman's pelvic cavity. The issue with CV lies in the overgrowth of Lactobacillus, resulting in an excessive production of acid. Excessive use of baking soda can completely eliminate Lactobacillus. When women lose this crucial first line of defense, it can increase the risk of pelvic infections, potentially leading to PID.
Instead of completely eradicating vaginal Lactobacillus, an effective CV treatment should aim to reduce the overgrown Lactobacillus to a more moderate level. This approach can help alleviate CV symptoms while ensuring the presence of a reasonable amount of vaginal Lactobacillus, which is essential as a protective health defense system for women.
CV-Ease: The First Dedicated Self-Care Product for CV Management
For women seeking alternatives to traditional home remedies like baking soda, CV-Ease offers a specialized approach.
Typically, vaginal lactobacillus bacteria act as a protective barrier against various infections. Managing CV effectively involves maintaining these beneficial bacteria while moderating their levels, rather than eliminating them. Overusing remedies like baking soda can disrupt this balance, potentially leading to unintended outcomes.
When the protective lactobacillus bacteria are reduced, the vagina may become more susceptible to infections. CV-Ease is designed to offer a gentler solution. Unlike baking soda or antibiotic creams, it works by neutrally buffering the lactic acid associated with CV and moderating, not eliminating, the lactobacillus bacteria. This helps maintain a balanced vaginal microbiome. CV-Ease is formulated from all-natural, food-grade ingredients, prioritizing safety without the use of harsh antiseptics.


NeuEve CV-Ease is the first specialized self-care product designed to provide relief for Cytolytic Vaginosis (CV). It may also be effective for addressing vaginal lactobacillosis (VL), as VL shares similarities with CV. You can now find CV-Ease available for purchase on both Amazon and our NeuEve website.
How to clear Lactobacillus iners?
However, there is one exception to note: Lactobacillus iners-associated CV presents a unique challenge. Lactobacillus iners, within the Lactobacillus family, has a tendency to cause infection by releasing a cytolytic toxin known as inerolysin. This bacterium is facultative and gram-positive. Neither BV Clear nor CV-Ease is equipped to provide relief in such cases. However, AV-NIL has shown promise in providing relief, possibly due to the bacterium's facultative nature, making its infection resemble that of Aerobic Vaginitis (AV).

Disclaimer: This article is for information purposes only. It is about natural products, nutrients, and/or methods for managing vaginal discomfort (not a true infection or disease). It is not medical advice for the treatment of any diseases.
*************************************************************************************
Customer feedback after using AV-NIL for L. iners-associated CV
Helped me cure vaginitis
Customer feedback after using CV Ease
"The product helps me so much I really wish I could use it every night! The symptom relief I have the day after is more than anything else has given me. Obviously I have hope this is going to work bc I keep purchasing more! I’m not sure what the other ladies are saying or how long they’ve had CV. I was diagnosed in August but believe I had CV since June. I just don’t think after having the condition for almost 7 months that 9-12 days of treatment are going to cure me. Does that make sense? Slow and steady wins the race is how I look at it and I fully believe I need to receive treatment nonstop for quite sometime to overcome this imbalance. That is why I would love to see it be used more often & for longer. I can’t help but feel like if I used it more frequently & for a lengthy duration that it would end this mess bc again, this product is AMAZING!"
"The CV-Ease product has definitely improved my cytolytic vaginosis symptoms. I feel clean and have no symptoms of cytolytic vaginosis as of today. I am clear! The CV-Ease side effects for myself were a very light itch nothing unbearable and the suppository discharge. I did not experience burning either irritation. The experience has been a positive one for me and I can finally say I feel free and clean! I am happy as a customer and glad to express that I purchased two CV-Ease packs to have one as a backup in my refrigerator. Thank you for creating the product, Dr. Renjie Chang!"
"Thank youuu! It is a lil irritation so I’m gunna continue the half suppository every other day![]() but I’m noticing no cottage cheese discharge anymore so that’s definitely a good sign! Thank you Renjie! You are a life saver
but I’m noticing no cottage cheese discharge anymore so that’s definitely a good sign! Thank you Renjie! You are a life saver ![]() ."
."
"I am currently using this product and I will smell it for 2 days after. It’s not an unpleasant odor, just slightly herbal in my opinion. I too have received AMAZING results since starting use on December 13. I am eager to see if I have even less symptoms as I enter into a second full monthly cycle. So very thankful for this product!"
"Okayy perfecttt thank you so much!! Very happy with the product so far! 💕 Have a blessed day!"
"Hello! Wanted to let you know I’m over a month out and have had 2 periods without any treatment and my CV is still kept at bay!! I do still have CV-Ease in the fridge in case I need it. :)"














Need help it hurts when I have sex and it’s real dry down there
This product seems amazing, but it is so expensive and thus inaccessible to many women who might have CV, including myself. Please please consider lowering the price so more people can use your product and get relief
I wish I could get it.am so desperate .the product is not available in my country. Please help .I feel like am dying with itchness and burn
Is there a way to order CV ease not from Amazon it does not ship to Canada
What is your recommendation for CV if you are sensitive to coconut oil? All of your products have it!
My situation is hard, because my biome test shows 99%lactobacillus overgrowth and shows a 1% ecoli. Plus I am post menopausal with atrophy. Just started estrogen therapy. So I have every indicator for AV, CV and VL!
I’d love to use your product, but for the coconut oil! :(
I am going to have to try the baking soda sadly.
Leave a comment