Bacterial Vaginosis : A Complete Overview

Vaginal Clue Cells coated with Gardnerella Vaginalis,
a bacteria is responsible for about 80% of BV cases.
Table of Contents
What is BV?
Bacterial vaginosis is an overgrowth of bacteria normally present in the vagina.
It's a polymicrobial condition, meaning there are many different bacteria involved and responsible.
In other words, it's a disturbance of the normal vaginal ecosystem.
Specifically, BV involves a high concentration of anaerobic bacteria.
Implications
BV has a moderate to severe impact on women
Nearly all women (>95%) report a negative impact on their sex life.
Women report feeling self-conscious, embarrassed, and overall uncomfortable in social situations. They say they think that everyone can smell them. It really impacts their quality of life.
BV is associated with:
- Preterm birth, pregnancy loss
- Intrauterine infections
- Postpartum, post-abortion endometritis
- Pelvic Inflammatory Disease and Sexually Transmitted Infections
Co-Infections of BV
All the STIs are intertwined with BV
Absence of lactobacilli and/or presence of BV associated with increased incidence of gonorrhea, chlamydia, trichomoniasis, syphilis, HPV, HIV, HSV, candidiasis, PID
BV makes HIV more likely
- Increased incidence of BV in women with HIV
- Increased transmission of HIV to women with BV
- Increased risk of female-to-male HIV-1 transmission in women with BV
- Increased viral shedding of HIV-1 in women with BV-associated bacteria (BVAB)
Prevalence
Did you know that BV is the single most prevalent symptomatic vaginal infection? It results in over 10 million office visits annually. It affects ~30% of US women of reproductive age. Interestingly, the majority of women do not report their symptoms.
Risk Factors for BV
The following is a list of the different social, medical, and sexual factors that are correlated with increased risk of BV. These factors don't cause BV, but they increase the risk of getting bacterial vaginosis.
Social Risk Factors
- Smoking
- Low Social Economic Status
- Poor Diet
- Obesity
Medical Risk Factors
- Douching
- Previous History of BV
- Hypoestrogenic Stage (having low estrogen), which may require natural treatment for vaginal dryness
- Abnormal Uterine Bleeding
- Antibiotic Usage
Sexual Risk Factors
- New partner
- Female partner
- Multiple partners
- Young age at first coitus
- Uncircumcised male partner
Symptoms of BV
First of all, many women are asymptomatic for BV. For women who do have symptoms, the most common symptoms are:
- A thin, gray, homogenous discharge that adheres to the vaginal wall
- "Fishy" odor
Some of the less common symptoms of BV are:
- Vulvovaginal irritation
- Vaginal itching
- Vaginal burning
- Dysuria (painful urination)
- Dyspareunia (painful sex)
The Healthy Vaginal Ecosystem
Every woman's vagina naturally has an ecosystem with bacteria. A healthy vagina is a very acidic environment. The vagina is actually one of the most acidic organs in the body! The pH should be in the range of 3.8-4.2, which is about as acidic as orange juice.
Lactobacilli (the same bacteria in yogurt) should be the dominant species of bacteria in a healthy vagina. Vaginal Lactobacilli produces hydrogen peroxide and lactic acid. This helps maintain a low pH and is thought by experts to be protective against HIV and other STIs.
Amsel Criteria
The Amsel Criteria is one way to officially diagnose Bacterial Vaginosis. In order diagnose BV, 3 of the following 4 conditions must be met:
- Homogenous thin, grey/white discharge
- Positive whiff test (smells like fish) either before or after using 10% KOH (potassium hydroxide)
- High vaginal pH of >4.5
- Vaginal clue cells on microscopy
Some people mistakenly believe that the presence of Gardnerella is enough to diagnose BV. However, for some women, Gardnerella is actually part of their healthy ecosystem! The presence of Gardnerella alone is NOT enough to diagnose BV.
Self-Collection of Vaginal pH
When self-collecting vaginal pH, patients usually make small errors. On average, a patient interprets their pH to be 0.2 points lower than it actually is. So if a patient interprets their pH to be 4.3, on average it's actually 4.5.
It's generally a good idea for women to self-collect their vaginal pH before seeing a doctor to save time and money.
Summary: This means if you measure your own pH and it's over 4.3, observe a thin, white/grey discharge, and notice a fishy smell, there's a very good chance that you have BV.
BV Treatment
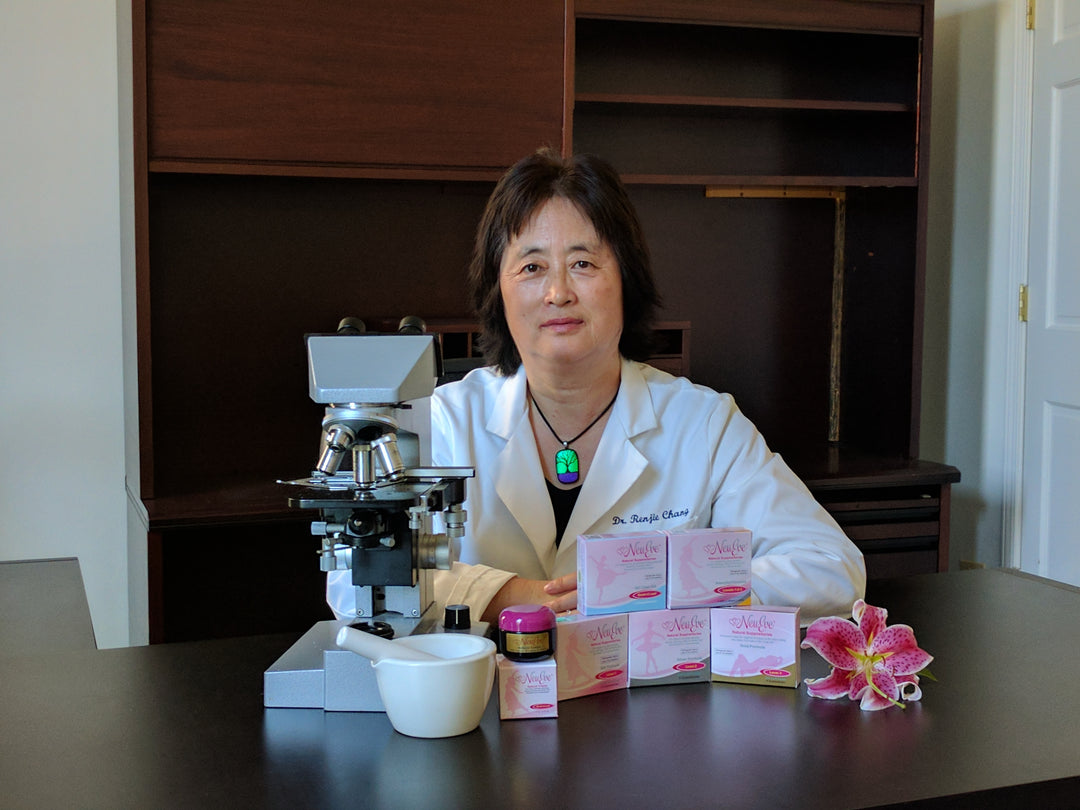
There are a lot of ways people treat BV, from official medical treatments, alternative medicines, and home remedies. Below we will start with the official CDC Guidelines for treating BV, then explain how NeuEve works in conjunction with the CDC recommended guidelines.
1st Line BV Treatment - from CDC guidelines
- Metronidazole (Flagyl) 500 mg taken orally, twice a day x 7 days*
- Metronidazole (Flagyl) gel 0.75%, 1 applicator (5 g) applied vaginally, once a day x 5 days*
- Clindamycin (Cleocin) cream 2%, 1 applicator (5 g) applied vaginally, every night at bedtime x 7 days
*For metronidazole, it's important to avoid ALL alcoholic beverages until at least 72 hours after the last use. Consuming even a tiny amount of alcohol while on metronidazole will cause you to become very, very sick.
These are the first-line medical treatments for non-chronic BV, so they are the ones most likely suggested by your doctor. One thing to keep in mind is that taking antibiotics will also wipe out the healthy bacteria in your vagina. Using NeuEve after antibiotics will help ensure the natural healthy vaginal lactobacilli are restored, similar to how vaginal probiotics work.
People often ask about metronidazole (flagyl) resistance. Here's a fact that might surprise you:
BV has a 70% resistance rate to metronidazole, which is why many women seek bv treatment online.
2nd Line BV Treatment - from CDC guidelines
- Tinidazole (Tindamax) 2g taken orally, once a day x 2 days
- Tinidazole (Tindamax) 1g taken orally, once a day x 5 days
- Clindamycin (Cleocin) 300 mg taken orally, twice a day x 7 days
- Clindamycin (Cleocin) ovules 100 mg intravaginally once at bedtime for 3 days*
*Latex condoms may be compromised within 72 hours after using clindamycin ovules.
These are the second-line medical treatments for BV. Generally, a physician will choose one of these choices if it's very important for the patient to consume alcohol.
Secnidazole (Solosec)
Secnidazole is a new antibiotic that was approved by the FDA in September 2017. It will be available very soon. The main difference secnidazole and existing treatments is that it's a single-dose, granule formulation. So you would mix it into soft food like yogurt, pudding or applesauce. Because it's very new, CDC guidelines haven't yet been updated to include secnidazole.
BV Treatment During Pregnancy and Breastfeeding
BV is associated with preterm birth and low-birth weight babies. For this reason, it's very important treat BV in pregnant women. Here's the key things you need to know about treatment for pregnant women:
- Avoid tinidazole
- Oral and vaginal metronidazole and clindamycin appropriate
Treating breastfeeding women with BV:
- BV causes no harm to infants
- While the mother is on antibiotics, defer breastfeeding until 24 hours after the last antibiotic treatment. Antibiotics go into the breastmilk.
- NeuEve should be used to treat BV for breastfeeding mothers, since NeuEve is all-natural and organic. NeuEve is perfectly safe for children.
Recurrent BV
After treatment with the first-line therapies, there are very high recurrence rates of BV.
Over 50% of women get BV again within a year of treatment.
It's very difficult to "cure" recurrent BV because there's an underlying shift in the vaginal flora. Once someone has recurrent BV, there's an 80% chance for it to come back.
Risk Factors associated with Recurrent BV
- Past history of BV
- Regular sex partner
- Female sex partner
- Abnormal vaginal flora
- Use of hormonal contraception
Treatment of Recurrent BV
According to the CDC, there's 4 steps to treating recurrent BV:
- Treat the current infection using CDC guidelines
- Suppression/prevention using one of the following:
- Metronidazole gel vaginally 2 times per week, up to 6 months
- High-dose metronidazole (compounded 750 mg per vagina x 7 days) has a higher cure rate than 500-mg dose
- Boric acid 300- to 600-mg vaginal capsules every night at bedtime x 2 weeks, then 2 times per week (also antifungal). Some women prefer boric acid alternatives for treatment.
- Probiotics (we recommend Fem Dophilus)
- Acidify the vagina (we recommend using NeuEve)
Many women who had long-term, chronic, recurrent BV were actually able to cure their BV by using NeuEve or a vaginal suppository for bv. NeuEve works by bringing the pH down to very low levels, and by providing vitamins and essential oils to the vagina tissues and vaginal ecosystem.
Common Questions
Is there a relationship between BV and condom use, or between BV and semen? Every time my partner doesn't use a condom, my BV comes back.
Answer:
The bacteria that cause BV are very sensitive to the vaginal pH. The normal vaginal pH is very acidic, and semen is very alkaline. When semen is ejaculated, it causes a pH shift in the vagina, which can cause BV to come back.






















Hello I felt off down there and went to doc for vaginal swab. Diagnosis gardnerella BV. But my symptoms are not clear cut. I have a bit more discharge which is slightly white/very light yellow. No odor whatsoever and burning sensation. First round of flagyl did not help.
Can I use NeuEve Gold as a preventative measure vaginal imbalance/BV while pregnant? I used to use one 600mg suppository of boric acid after unprotected intercourse as a prevention & it worked great for me with no recurrence of BV. I haven’t had any issues in years and now I’m wondering what I can safely use to replace my old preventative routine.
Hi Dr. Chang, I am 45 years old and am experiencing recurrent BV for the first time. I think it may have something to do with my age (and drop in estrogen, perhaps?) I struggled with chronic yeast infections when I was younger, but that resolved itself once I discontinued the use of oral contraceptives. I am infertile (I assumed it was due to the almost non-stop yeast infections and cervical inflammation I was told I had, but was never told a reason), so do not use condoms. I enjoy an active sex life with my long-time boyfriend. He is uncircumcised, but I’m having a hard time considering that as a factor because a) he always cleans himself before sex and b) for the first few years we were together, my vaginal health was perfect! He would even comment on how I had zero smell. I use the Silver formula with good results (usually just one dose and it’s good to go), but I’m struggling to understand why now I feel like BV rears its ugly head following every episode of sex. Using condoms isn’t really an option for us, is there any hope for me??
Thank you in advance for your help.
Sara Johnson
Hi, i am having my second BV treatment (last one was 5 years ago), and having a few yeast infections in between (2 per year maybe) – how to ensure a good PH level or prevent non-balanced vagina flore? I know there is pro-biotics but they are usually cure of 30 days. So should we do few cures a year? thanks a lot
Dr. Chang,
I have recurrent BV-atopobium vaginae and a ureaplasma infection resistant to antibiotics that I’ve struggled with for six months. What supplements do you recommend starting with? Thank you!
Leave a comment