Top Strategies to Relieve Menopausal Dryness Naturally
What is menopause?
According to the US National Institute on Aging (NIA) of the NIH and the World Health Organization (WHO), menopause is not a disease; it is a natural stage of a woman's life.

A series of papers published in the Lancet recently reveals how drug companies profit from portraying menopause as a “disease,” leading to misinformation and ineffective treatments of hormonal drugs for women.

Hormones have health risks

Overmedication is a public health concern
The World Health Organization views overmedication as a significant public health concern, contributing to millions of global hospitalizations due to adverse drug reactions and accounting for billions of dollars in unnecessary healthcare expenses.
Estrogen supplementation may provide short-term relief, but it has long-term consequences. It not only increases healthcare maintenance costs but also elevates the risk of numerous diseases, including heart disease, stroke, thrombosis, gallbladder diseases, uterine fibroids, and breast and uterine cancers.

Drug companies attempt to downplay the risk of estrogen in causing breast cancer, but recent research from scientists at Harvard has revealed that estrogen not only increases the risk of developing breast cancer but also directly contributes to its onset. This alarming discovery underscores the urgent need to explore safer and more effective alternatives to estrogen to safeguard women's health.
Safer and more effective products
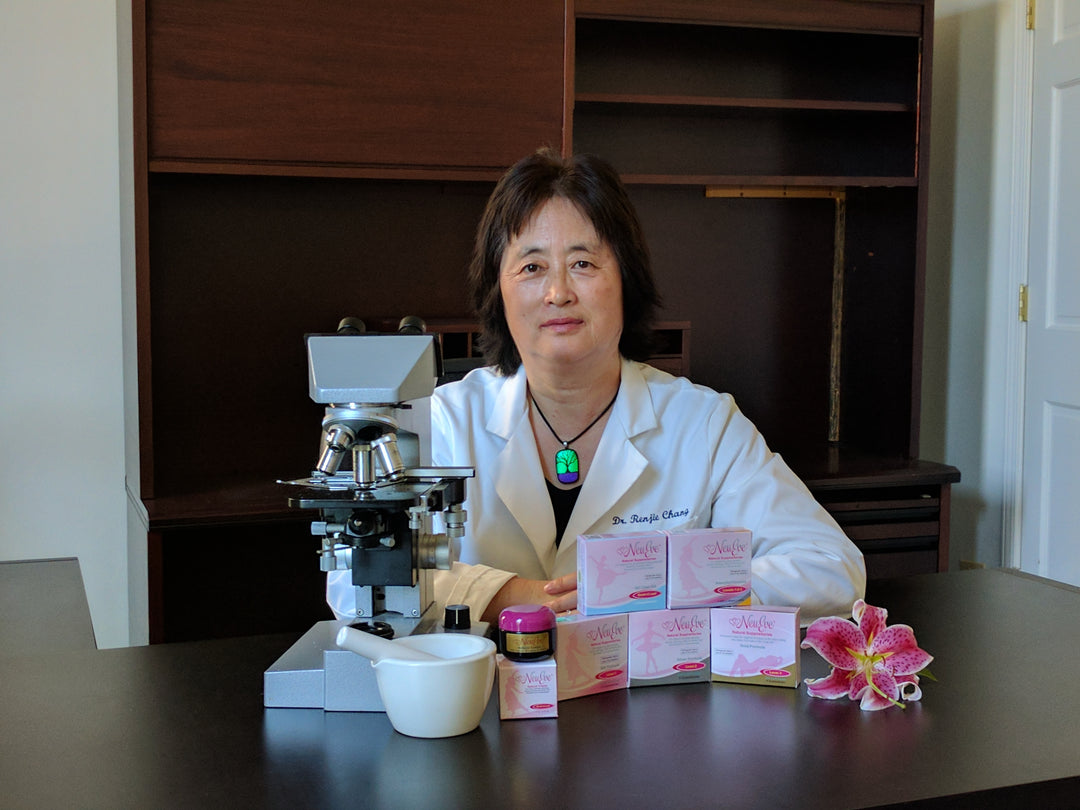
NeuEve offers a safer and more effective premarin cream alternative to estrogen. It is not a drug but a food-grade natural product.
To date, NeuEve has helped over 100,000 women find relief safely from menopause-related vaginal dryness, including many who tried estrogen unsuccessfully and breast cancer survivors who cannot use estrogen.

Vaginal moisturizer NeuEve, a scientific breakthrough in women's health, effectively and safely relieves menopause-related vaginal dryness without the need for hormones.
This article explains how NeuEve works.
Disclaimer: This article is for informational purposes only. It discusses natural products, nutrients, and alternative methods for managing discomforts associated with vaginal dryness (not a true disease). It is not intended as medical advice for the treatment of any diseases.














Leave a comment