Painful sex and endometriosis

If you have read my personal blog on our homepage, you will know that one of my primary goals in creating NeuEve was to help couples navigate the challenges that can arise over many years of marriage.
As Lucy, one of our ambassadors, mentioned in one of her videos, ending up in a roommate-like situation with your spouse is not the ideal outcome for most marriages. In my research on painful intercourse, I came across endometriosis, which can cause significant discomfort during menstruation and is a common reason for painful sex, medically referred to as dyspareunia.
Unfortunately, traditional medications may not always provide relief from this sexual pain. Moreover, hormonal therapy drugs often used to manage endometriosis might lead to other issues like vaginal dryness and discomfort during intercourse. This further motivated me to explore natural methods that could support women experiencing these symptoms.
What is Endometriosis?
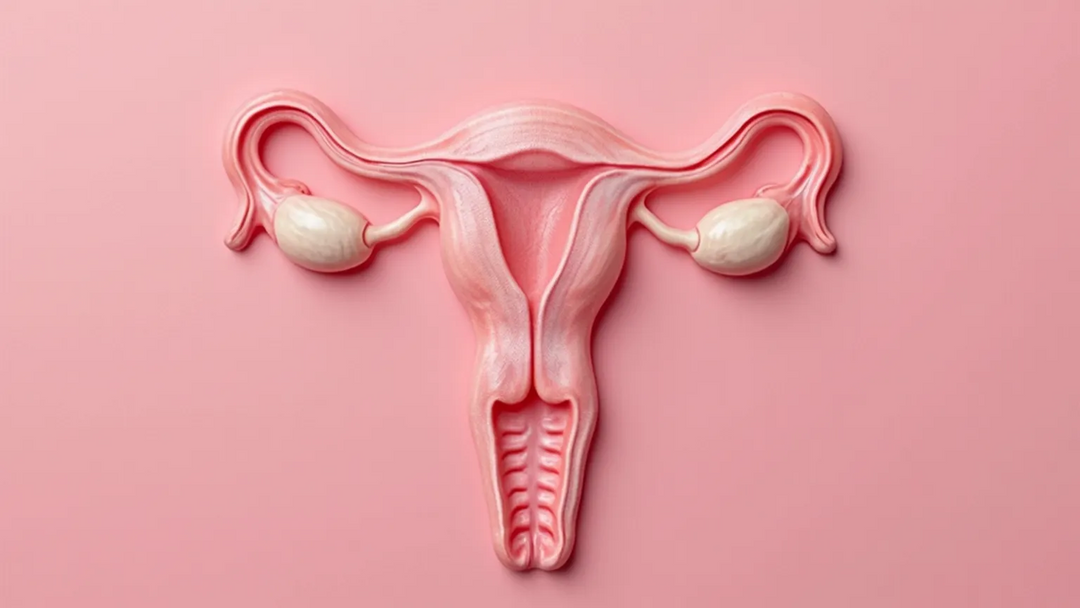
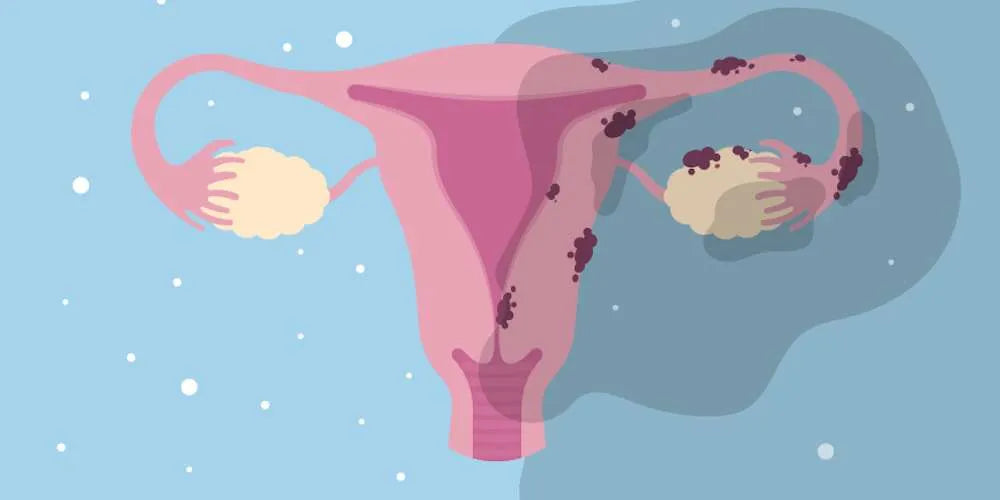
Endometriosis is a condition where tissue similar to the lining inside the uterus grows in other places, such as the ovaries, fallopian tubes, and the lining of the pelvis. Sometimes, it can also affect the intestines and urinary tract. Think of it like the roots of a tree spreading beyond their intended garden bed. Here, tissue that should be confined to the uterus grows in areas where it isn’t supposed to be.
Many of us might know someone with cysts; it's quite common and related to this condition. In cases of endometriosis involving the ovaries, the dislodged tissue may bleed and lead to the formation of an ovarian cyst, comparable to traffic jamming up in a narrow alley, creating a blockage.
For more information about endometriosis, you can visit the Endometriosis Foundation website.
 Endometriosis – the lining tissue grows outside the uterus
Endometriosis – the lining tissue grows outside the uterus
You are not alone: Endometriosis is a collective experience
Numbers don’t lie. Endometriosis affects 10–15% of all women of reproductive age and 70% of women with chronic pelvic pain. Although many women need help, the delay in diagnosing endometriosis is very alarming. Unfortunately, this can result in unnecessary suffering and a considerably reduced quality of life.
1 in 10 women of reproductive age (15-49 years) deals with Endometriosis
176 million women today suffer from Endometriosis
Pay Attention to the Symptoms
At this point, we understand that endometrial tissues can be misplaced due to endometriosis. During menstruation, these displaced tissues may swell, break down, and bleed. This is not only painful in theory but can be intensely painful in practice, often exacerbating the discomfort typically associated with menstrual periods.
Recall the analogy of the trapped cars without an exit? Similarly, when bleeding from these misplaced tissues has no exit, the blood becomes trapped. Trapped blood can lead to irritation, inflammation, and potentially to scarring and adhesions in the surrounding tissues.
These endometrial scars or adhesions may cause the uterus to adhere in a backward position, akin to being slowly glued in place. Unfortunately, this situation might contribute to the development of a retroverted uterus.
Symptoms may include:
- Chronic pelvic pain
- Severe pain in the pelvis
- Increased pain during menstrual periods, bowel movement, or sexual intercourse
- Fertility may also be reduced.
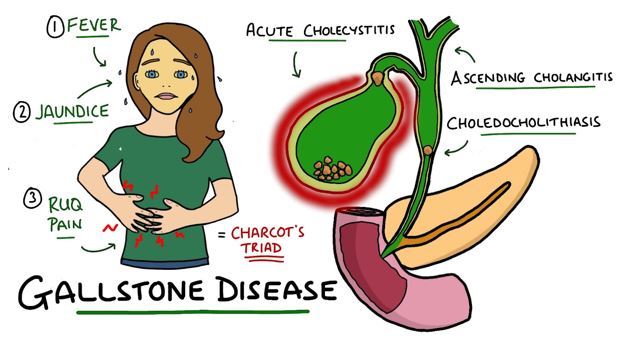
In addition to the fact that endometriosis is often overlooked, due to the severe pain in the pelvic floor it is commonly misdiagnosed as pelvic organ prolapse, interstitial cystitis, pelvic inflammatory disease, or irritable bowel syndrome.
Interesting fact: To achieve a precise diagnosis, researchers are developing a smart tampon. Once developed, it will hopefully be able to diagnose endometriosis from menstrual fluid extracts.

HOW IS ENDOMETRIOSIS PAIN MANAGED?
We can have a very extreme “solution” for severe endometriosis: surgery. The lesions can be removed, like hysterectomy and laparoscopic surgery. However, most women with a mild case manage the condition by non-surgical options. For endometriosis pain management, your doctor may recommend or prescribe the following medication:
1) Painkillers
- Over-the-counter painkillers (like ibuprofen, acetaminophen, naproxen)
- Prescription-strength painkillers (like ibuprofen, naproxen)
- If the pain is not controllable by the above medications, opioids may be prescribed (like hydrocodone with acetaminophen).
2) Hormonal therapy
- Hormonal birth control (like pills, injection, implants, IUDs)
- Gonadotropin-releasing hormone antagonists (like Orilissa)
- Androgenic hormones (like danazol)
- Aromatase inhibitors: Arimidex (chemical name: anastrozole), Aromasin (chemical name: exemestane), and Femara (chemical name: letrozole).
Painkillers may not work well for painful sex.
But what about painful sex? Let's be clear, sexual health is important—it contributes to our happiness and well-being. However, certain treatments for endometriosis, such as hysterectomy or hormonal therapy, can lead to vaginal dryness and atrophy, which in turn may cause discomfort during sex, decreased libido, and challenges in sexual function.
Painful Sex and Endometriosis: A Challenging Combination
It’s crucial to understand that endometriosis can affect various areas around the uterus, fallopian tubes, and the back of the vagina, which is why the experience of sexual pain may vary.
For example, if endometriosis affects the area behind the vagina or the lower part of the uterus, it can make sex extremely uncomfortable, a condition known as deep dyspareunia.
In cases where endometriosis grows between the vagina and the rectum, it can lead to the formation of scars or adhesions. During penetration, these adhered tissues may be stretched or pulled, causing pain.
Alternatively, if the endometriosis is located on the ovaries, the pain during sex might be less intense or not occur at all. However, if it spreads across multiple pelvic organs, including the uterus, the discomfort during sex might increase.

Endometriosis may cause painful sex
Some women consider options like hysterectomy or hormone therapy to manage their endometriosis. A common concern with these treatments is that they may lead to lower estrogen levels, which in turn can cause vaginal dryness and make sex uncomfortable.
Challenges of Endometriosis Treatments in Relieving Painful Sex
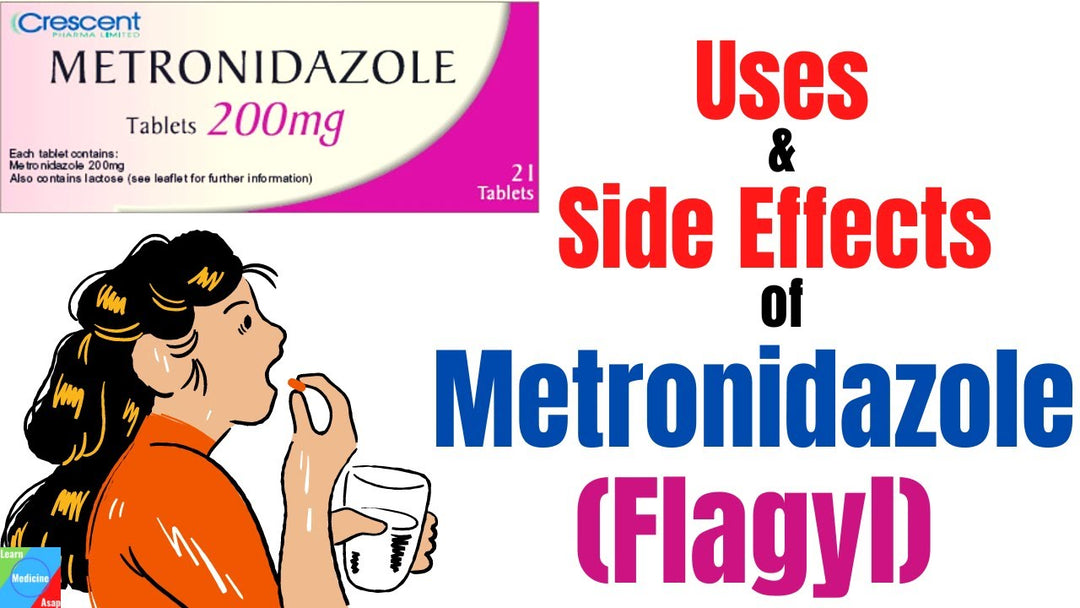
It is well-recognized that painful sex can be a problem for women with endometriosis due to the presence of inflamed tissue. While anti-inflammatory medications might be considered to manage inflammation, they may not be effective for all causes of pain during sex.
Often, discomfort during intercourse can also result from the stretching of scars or tissue adhesions formed from previous tissue damage related to endometriosis. Since these issues do not necessarily involve active inflammation, anti-inflammatory medications might not address the pain associated with this specific condition.
Treating endometriosis with hormone therapy or hysterectomy may cause vaginal dryness, shrinking, or painful sex.
Estrogen is often recommended to reverse vaginal dryness and atrophy, but this can increase the severity of endometriosis. Therefore, estrogen shouldn’t be used to relieve painful sex in women with endometriosis.

Drugs may not ease painful sex in women with endometriosis.
Natural Support for Women with Endometriosis and Discomfort During Intimacy
In a world full of chemicals, embracing nature can be a refreshing change. For those looking for alternatives when estrogen is not an option, natural solutions might be considered.
NeuEve may be seen as one such alternative. It is designed to nourish vaginal tissue using ingredients sourced from nature. It also includes ingredients known for their soothing properties.
To date, many women experiencing severe vaginal dryness, including those with endometriosis, have shared positive feedback about their experiences with NeuEve cream and suppositories.
For women experiencing vaginal dryness, deep pelvic discomfort, and discomfort during penetration, incorporating dilation exercises might be beneficial. These exercises can help by gently stretching the tissues, which may support the natural process of maintaining tissue flexibility. This can also contribute to the overall comfort of the vaginal area.
Many of our customers reported excellent results using NeuEve together with a vaginal dilator. We recommend the VuVa Smooth Set of Five Dilators, and the VuVa Neodymium Magnetic Set. These are higher in price, but you’re really getting what you pay for. They are worth it!
These dilators are not our products. They are sold by VuvaTech. For convenience of our customers, we list the product links below:
Buy Non-Magnetic Pelvic Dilators
Tips about using dilators:
1) Avoid overstretching. It is understandable that one may wish to move up the sizes quickly to get a more rapid recovery. However, this can be counterproductive. The recovery of vaginal atrophy is a slow process. Moving up the dilator sizes too quickly or skipping sizes can cause overstretching, which in turn can tear the atrophied tissue to cause injuries. Please do not skip the sizes and try the largest dilator first. Please be patient and do the exercise with a stepwise increment to avoid possible injuries due to overstretching. Please give one size dilator at least 3-4 weeks to allow the tissue to catch up with the growth before moving up to the next size.
2) Preventing UTI. Physically, dilation exercise is like sexual intercourse. The penetration movement can mobilize bacteria normally on the skin into the bladder to cause UTI. You will need to pee immediately after each exercise to prevent UTI. Urination can flush out any bacteria that entered the bladder during the dilation exercise. Therefore, drinking a lot of water before exercise helps build up the urinating flushing pressure and prevent UTI. If you are dealing with UTIs, you may find support on NeuEve Corsaria, our daily supplement for urinary tract health.
Disclaimer: This article is for information purposes only. It is about natural products, nutrients, and/or methods for managing vaginal discomfort (not a true infection or disease). It is not medical advice for the treatment of any diseases.











Yes, endometriosis can continue to grow after a hysterectomy if one or both ovaries are left intact. Since this tissue is estrogen-sensitive, it can still respond to estrogen produced by the ovaries. Consequently, symptoms of endometriosis may persist or recur post-surgery. For those still experiencing symptoms with ovaries intact, treatment options include hormonal therapies to suppress estrogen, pain management, or potentially removing the remaining ovarian tissue. It’s crucial to consult with a healthcare provider to customize the treatment plan based on individual needs.
Can endometriosis continue to grow after having had a hysterectomy if they left one of my ovaries? I had severe endo when I was younger and had multiple surgeries to remove it before finally getting the hysterectomy. I have terrible pain with intercourse and atrophy for sure. I’m almost done with my first month of NewEve and I think it’s helping. I’m excited to keep trying but was just curious if this could be part of my problem.
Leave a comment