Sex After a Hysterectomy (and Advice for Husbands)

If you are a woman (or her husband) and worried about sex after a hysterectomy, this article is for you! In this article we will discuss how the different types of hysterectomy affect your sex life, how long to wait to have sex, and what happens to hormone levels, libido, and sexual function.
What is a Hysterectomy?
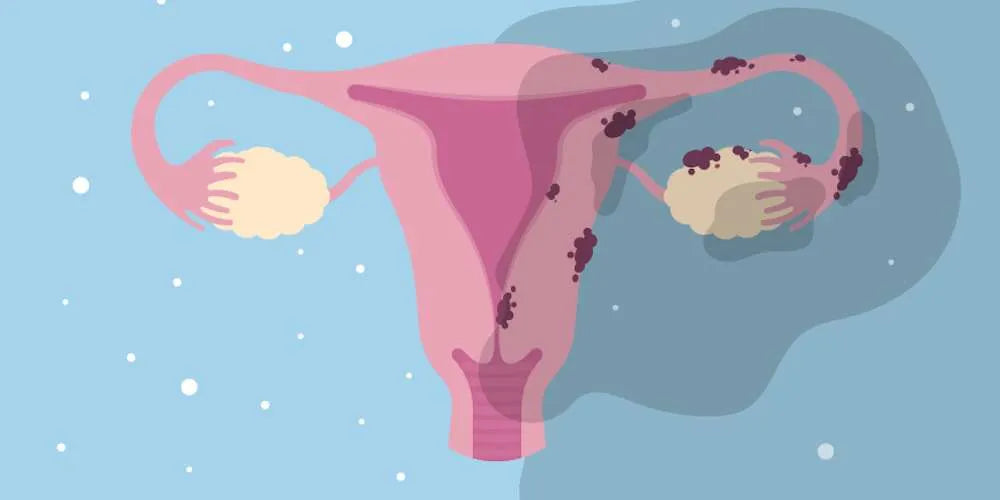
It's a surgical procedure to remove the uterus, often employed to treat conditions like fibroids, endometriosis, and various cancers.
How does a Hysterectomy affect sex life?
It depends on what type of hysterectomy: partial hysterectomy (only uterus removed) or bilateral oophorectomy (both ovaries removed).
How does a Partial Hysterectomy (only uterus removed) affect sex?
Generally, if only the uterus is removed, it might not significantly affect sexual activity in the long term.
How soon can I start having sex after a partial hysterectomy?
It’s recommended to refrain from sex for about six weeks post-surgery to allow for healing. After this period, many resume their sex life.

How does a Bilateral Oophorectomy (both ovaries removed) affect sex?
About 50% of hysterectomies include the removal of the ovaries, especially in cases involving cancer.
Why remove the ovaries? Do hysterectomies affect libido?
Though vital for hormone production, ovaries might be removed to reduce the risk of hormone-sensitive cancers. This drastically reduces estrogen levels, leading to changes like vaginal dryness, decreased libido, and possible painful intercourse.
What Happens to Estrogen Levels and Testosterone Levels after a Hysterectomy?
Post-hysterectomy, especially after oophorectomy, you might face a significant drop in estrogen and testosterone. Estrogen is crucial for maintaining healthy reproductive tissues, while testosterone is linked to libido. Therefore a lack of estrogen or testosterone results in vaginal atrophy (shrinking and drying of the vaginal tissues) and a decreased sex drive.
Can I take Estrogen Replacement Therapy?
It’s generally not advised to supplement estrogen post-hysterectomy due to the increased risk of hormone-sensitive cancers. This presents a dilemma for those seeking relief from menopausal symptoms post-surgery.

Can I take Testosterone Replacement Therapy?
While testosterone has been explored for treating sexual dysfunction, its effectiveness is limited, and the potential side effects are significant.
Tips for Sex after a Hysterectomy: What are Non-Hormonal Options for Restoring Sexual Tissues and Libido?
Fortunately, there are non-hormonal methods available that can support women facing sexual dysfunction post-hysterectomy:
-
Vaginal lubricants and moisturizers
-
Vaginal dilators
-
Non-invasive treatments like laser therapy
-
NeuEve (which works by topical nourishment)
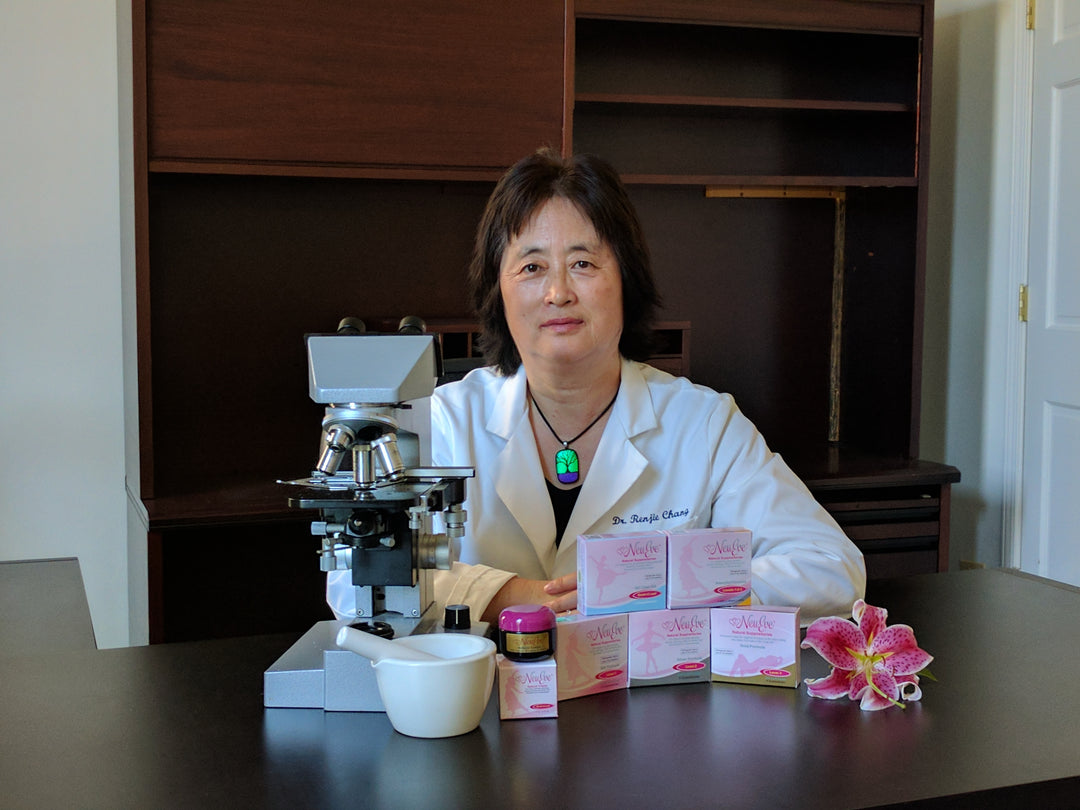
What is NeuEve and how does it work?
NeuEve is designed to support issues like painful sex and vaginal dryness using nutrients similar to how calcium and vitamin D support bone health. It's a safe, natural, and hormone-free option that has been positively received by many women, including those post-hysterectomy.
There is hope and potential for a fulfilling sex life after hysterectomy, and exploring these options can be a crucial step toward recovery and comfort.

How to manage stubborn vaginal dryness and painful sex safely?
How to manage vaginal dryness and painful sex for cancer survivors?









Sex is sooo painful that every time I try, I try to just take the pain and I can’t The skin around my vaginal entry is supper thin. It feels like if I had some super deep paper cuts. I’m giving up.
Dear Holly, I’m sorry that you’ve experienced this.
This is actually a very common story that we hear, in fact many of our customers after using NeuEve were able to regain their libido and vaginal wall integrity.
We are here for you.
My Hysterectomy was 10 yrs ago and I have not been with anyone since then, before the surgery My husband and I spoke with the surgeon telling him to leave my ovaries in tact unless it was absolutely necessary for example finding cancer then he was suppose to stop and explain that they found cancer and it’s important we remove everything but only if it was completely necessary but that never happened, he went ahead and removed everything leaving half a woman. I have “NO” sex drive and my husband divorced me now I used J&J Baby Powed/Talcum Powder before I had the surgery, I’m only in my 50’s and I feel like my life is over, I trusted the surgeon and now having “NO” desire for sex and other factors I hold the surgeon responsible because I never told him to take everything just a partial and now I’m I’ll and have a lot of medical problems and nobody to learn on or love me enough to deal with the amount of pain I’m dealing with!
What do you have to treat clitoris atrophy?
How soon after a total hysterectomy is it safe to use the silk suppositories and dilators? I used them for months before the surgery. A small section of the top part of my vagina was also removed. It should be healed in 4 weeks. Surgery was Jan 12, 2023.
Leave a comment